CASPR Technologies Named Finalist in 2026 AHR Innovation Awards

Visit us at AHR Expo 2026 in Las Vegas | February 2–4 We’re excited to share that CASPR Technologies has been recognized as a finalist in the 2026 AHR Innovation Awards, one of the HVACR industry’s most prestigious honors. Our recognition in the Indoor Air Quality (IAQ) category reinforces our mission: to make indoor spaces […]
Beyond Six Feet: Why Distance Alone Won’t Keep Us Safe from Airborne Diseases

The “six-foot rule” became a household phrase during the COVID-19 pandemic – simple guideline that promised safety from airborne diseases through distance. But as scientists have learned more about how respiratory diseases actually spread, this rule has revealed itself to be dangerously incomplete. The Science Behind the Spread of Airborne Diseases When we breathe, speak, […]
The Invisible Threat: Why We Can’t Rely on Symptoms to Detect Contagion

The human body is remarkably deceptive when it comes to infectious diseases. We’ve been conditioned to think of illness in terms of visible symptoms: the telltale fever, the persistent cough, the runny nose that signals it’s time to stay home. But this symptom-centric view of contagion represents a dangerous blind spot in our understanding of […]
ASHRAE 2025: The Future of Indoor Air Quality is Taking Shape

A few weeks ago, I joined several thousand colleagues in Phoenix, Arizona for the ASHRAE 2025 Annual Conference, one of the two pivotal meetings where the organization conducts its most important business. This year’s conference felt particularly significant as we welcomed our new President, Bil McQuade, and his compelling theme for the 2025-26 ASHRAE Society […]
Beyond Fresh Air: Why ASHRAE’s Ventilation Standards Need Active Air Cleaning

The COVID-19 pandemic fundamentally changed how we think about indoor air quality. Suddenly, terms like “air changes per hour” and “MERV ratings” entered everyday conversations. But as we’ve learned more about airborne pathogen transmission, a critical question has emerged: Is bringing in fresh outdoor air enough to keep us safe? Recent research suggests the answer […]
Bridging the Gap: How ASHRAE Standards Lead Building Codes and the Case for Early Adoption

The relationship between ASHRAE standards and building codes represents one of the most significant dynamics in modern construction and building performance. While building codes establish the minimum legal requirements for construction, ASHRAE standards often serve as the technical foundation that eventually shapes these codes. However, a critical lag time exists between when ASHRAE publishes updated […]
Understanding Pathogen Elimination: A Hierarchy of Resistance
Effective pathogen elimination and control is critical in healthcare settings, food safety, and water treatment. As the lab results demonstrate, different microorganisms exhibit varying levels of resistance to disinfection methods. This resistance hierarchy has important implications for infection prevention strategies. The Pathogen Elimination Hierarchy The test results reveal a clear progression from “easiest to kill” […]
The Hierarchy of Controls: A Systematic Approach to Pathogen Management
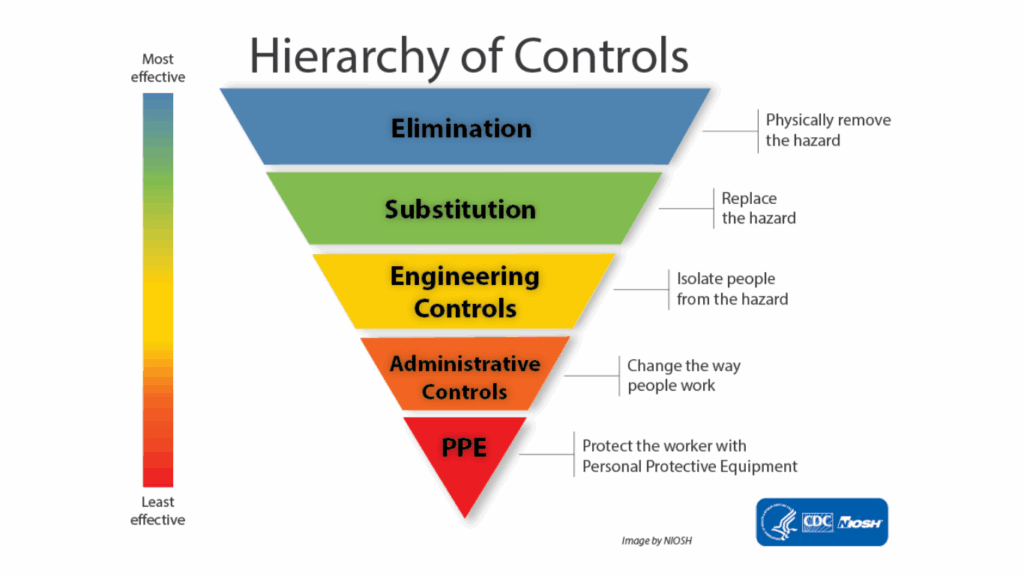
When it comes to protecting people from pathogens and other workplace hazards, not all control measures are created equal. The Hierarchy of Controls is a systematic approach that prioritizes the most effective strategies for preventing exposure to hazards, including infectious agents. What is the Hierarchy of Controls? The Hierarchy of Controls is a framework used […]
Breathe Easy: ASHRAE’s Guidelines for Better Indoor Air

Ever wonder what makes the air inside buildings healthy to breathe? ASHRAE publishes standards and guidelines for indoor air quality. Here’s what you need to know in plain language. What Are These Guidelines? Think of ASHRAE Standard 62.1-2022 as a rulebook for good indoor air in commercial facilities. It sets minimum requirements for ventilation (bringing […]
CASPR Technologies at AHR 2025: Elevating Indoor Air Quality in the HVAC Industry
The AHR 2025 conference in Orlando was an unparalleled experience for CASPR Technologies, bringing together industry leaders, innovators, and professionals from across the HVAC sector. The event served as the perfect platform for us to connect with experts, exchange ideas, and demonstrate how CASPR’s advanced technology is setting new standards for Indoor Air Quality (IAQ). […]
