CASPR, a One Health approach to combat any emerging pathogens indoors
In the US, One Health is an interdisciplinary approach to health usually focused in local and state public health departments, that encompasses a broad array of sectors, including public health, agriculture, animal and meat production, and environmental experts. The goal is to improve and encourage practices to improve health outcomes and reduce the threat of new, unknown pathogens, while containing exposure to the known pathogens. (1) CASPR technologies offers a comprehensive approach to improving health in our connected world by making indoor air safer, preventing spread of any new pathogen that emerges, as well as existing pathogens. Simply, CASPR is a prevention component for indoor buildings and facilities through a One Health lens.
We know that antibiotics are highly effective, with an estimated 5.7 million people (about twice the population of Arkansas) dying annually from treatable infections because effective antibiotics are not available to them. The problem is that antibiotics are overused, when they are improperly or inappropriately prescribed, and create antimicrobial resistance (AMR), in which antibiotics are not effective. About a quarter of all antibiotic prescriptions in the US are unnecessary. In addition, taking antibiotics for only a few days, or taking lower quality or the wrong antibiotics can have serious health consequences for the person and can create a path for drug-resistant organisms.
Outside of the US, lack of access to any antibiotic is a bigger problem in producing AMR. AMR is a global hitchhiker that does not recognize the borders of human, animal, and plant vulnerability. The astronomical cost of developing new antibiotics to keep pace with new mutations created with AMR is estimated to be about $1 billion (about $3.1 per person in the US) to develop 10 to 15 years to get through proper safety and efficacy testing to be marketed. Everyone is at risk from AMR, so preventing AMR by reducing indoor pathogens with a continuously active indoor room air cleaner is the best prevention from spreading pathogens indoors, known, and unknown.
In particular, improper use of antibiotics for humans that are given to animals accounts for AMR. It should be noted that more than 70% of new infectious diseases are zoonotic—that is a pathogen “jumps” from animals to humans, sometimes after mutations. Currently, many are keeping up to date on the latest news regarding Avian Flu (H5N1). Avian Flu has been recently detected in pigs, who happen to be closer to human genetics capable of spreading new respiratory pathogens than cattle or poultry. It is crucial to watch this in the coming weeks.
Without proper facility air and surface controls in animal and meat products, animal products can become contaminated and can spread resistant bacteria by food contamination. This can occur either by improper processing or cooking of animal products, or from fertilizer spraying of agricultural crops containing animal or human manure with resistant pathogens. While some producers still use human antibiotics in animals to promote growth, or in feed, these practices can result in the production of resistant organisms, and results in AMR. Therefore, AMR efforts within One Health should include livestock workers, farmers, and veterinarians, and a re-examination of pathogen reduction in air and surfaces, beyond intermittent surface cleaning or two-week fallow periods.
Evidence exists that antibiotic stewardship—a crucial One Health effort that ensures antimicrobials are used appropriately, only when necessary— reduces antibiotic consumption, slows drug resistance, and can be done without sacrificing patient and animal care. In a multicountry study, a 7-day course of antibiotics to humans can be equally effective against bloodstream infections as a 14-day regimen, and less likely to create resistant organisms. (2)
Reduction of risk from respiratory pathogens indoors is another key goal of One Health. Respiratory pathogens, like avian flu, seasonal influenza, colds, and Respiratory Syncytial Virus (RSV) are spread through the air. Measles is particularly efficient at spreading indoors, with a 90% risk of transmission to unvaccinated individuals.
While we all want to forget the years of confusion about the COVID-19 pandemic, some key lessons can be learned from the height of the pandemic. Infectious respiratory particles (IRPs) spread infection quickly from human to human, after “jumping” species from animals to humans. Now, COVID-19 is still with us, mutating, and is still circulating, with its newest variants. We are getting ready to hit prime seasonal influenza season, with a looming watch on avian flu, and other respiratory pathogens, like RSV, Simply, the COVID-19 pandemic taught us we need to be prepared and prevent infections indoors.
So how do you prepare and prevent infections indoors? We do not know who may be infected with pathogens inside the buildings where we work, play and live. People could be recently infected but asymptomatic, releasing IRPS continuously, and needing a continuous cleaning process to match the continuous release of those pathogens. A crucial One Health effort for antimicrobial stewardship promotes the appropriate use of antibiotics to humans, only when necessary, and this slows drug resistance, while assuring healthy outcomes of patients. Preventing spread indoors with CASPR prevents the spread of AMRs, too, consistent with One Health concepts.
AMR is an important One Health effort because of the global burden of antimicrobial resistance, now and in the future. In 2021, 4.71 global deaths were attributed to drug-resistant bacterial pathogens, directly responsible for 1.14 million deaths. (2, See also FIGURE 1, Reference 3) And this is expected to continue, with about a 70% increase in the number of annual deaths directly attributable to AMR by 2050, reaching 1.91 million in 2050. Within the next 25 years, more than 39 million people (about twice the population of New York) are predicted to die from antibiotic-resistant infections over the next 25 years. (2)
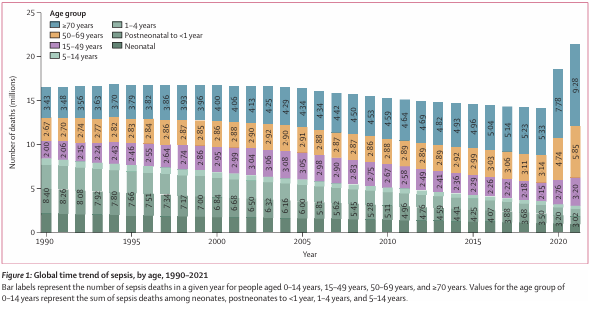
Figure 1, Reference 3
This is why continuously reducing IRPs in the air and on surfaces will help to reduce whatever pathogens emerge, as well as existing pathogens. In addition to antibiotic controls, facility control measures for continuous removal of indoor pathogens are a One Health approach, with CASPR’s continuously active indoor air cleaning.
CASPR is a One Health Strategy in Preventing Spread of AMR Pathogens
In September 2024, a global AMR conference was held. Just a few minutes before the start of this meeting, the prime minister from Barbados stated, “Imagine what happens if you get an infection from going into the garden or having a baby or going to the dentist…These are things that can bring your life to an end within 48 to 72 hours if the particular antibiotics that you’re using [are] not effective.” It seems like prevention of these AMR outbreaks with CASPR, a continuously active indoor air cleaner, is the continuous vigilance needed, consistent with a One Health approach to protection of humans, animals, plants, and the environment.
- Centers for Disease Control and Prevention (CDC) website. One Health. Accessed 11/24/2024 at About One Health | One Health | CDC
- American Medical Association, Medical News & Perspectives ed. Kate Schweitze Associate Managing Editor: UN Meeting Highlights Antimicrobial Resistance “Epiphany”—Lack of Antibiotic Access Is a Key Driver. Published Online: November 8, 2024. doi:10.1001/jama.2024.21
- GBD 2021 Antimicrobial Resistance Collaborators, Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050. Lancet, 2024; 404: 1199–22.